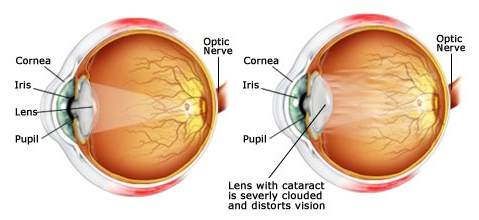

The lens, where cataracts form, is positioned behind the colored part of your eye (iris). The lens focuses light that passes into your eye, producing clear, sharp images on the retina — the light-sensitive membrane on the back inside wall of your eyeball that functions like the film of a camera.
How a cataract forms?
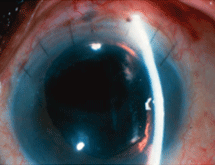
A cataract scatters the light as it passes through the lens, preventing a sharply defined image from reaching your retina. As a result, your vision becomes blurred. As you age, the lenses in your eyes become less flexible, less transparent and thicker. Age-related changes cause tissues within the lens to break down and clump together, clouding small areas within the lens. As the cataract continues to develop, the clouding becomes denser and involves a greater part of the lens. Cataracts may develop in only one eye, but they usually develop in both of your eyes. However, the cataracts usually aren't totally symmetrical, and the cataract in one eye may be more advanced than the other.
Symptoms:
1. Cloudy, blurry, fuzzy, foggy or filmy vision.
2. A noticeable cloudiness in the pupil.
3. Increased glare from lights eg: from headlights when driving at night.
4. A decrease in distance vision but an improvement in near vision.
5. Double vision (diplopia).
6. Frequent changes in glass power.
7. Impairment of colour vision.
8. Poor vision in sunlight.
Techniques of cataract removal
Extracapsular cataract extraction (ECCE) involves the removal of almost the entire natural lens while the elastic lens capsule (posterior capsule) is left intact to allow implantation of an intraocular lens. It involves manual expression of the lens through a large (usually ten to twelve mm) incision made in the cornea or sclera. It is very rarely done now a days only indicated for patients with very hard cataracts or other situations in which phacoemulsification is considered to have potential problems.
Disadvantages:
1. Long recovery period four to six weeks
2. Stitches are required
3. Need injection anasthesia
4. Higher risk of intraoperative complications
5. Higher incidence of postoperative astigmatism with increased dependence on glasses
6. Higher chance of posterior capsular opacification and need for laser capsulotomy
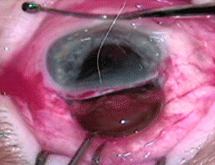
Manual small incision cataract surgery (MSICS): This technique is an evolution of ECCE (see below) where the entire lens is expressed out of the eye through a self-sealing scleral tunnel wound (five to six mm) . An appropriately constructed scleral tunnel is watertight and does not require suturing. The "small" in the title refers to the wound being relatively smaller than an ECCE, although it is still markedly larger than a phaco wound. The advantage of this technique is low cost.
Disadvantages:
1. Recovery period is about three weeks.
2. Need injection anasthesia.
3. Need injection anasthesia
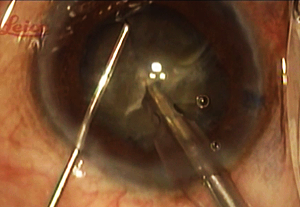
Phacoemulsification – A keyhole incision only two point two to two point eight mm wide is made on the outside of the eye. A circular opening in the lens capsule exposes the cataract. Next the phaco-emulsifier is inserted. This sophisticated instrument uses high-speed ultrasound waves to break the cataract into tiny pieces which are suctioned out of the eye.
Advantages:
1. Recovery time is two weeks leading to faster visual rehabilitation.
2. No injection required – done under topical anasthesia.
3. Minimal postoperative surgical induced astigmatism.
Types of IOL
Once you have made a decision to undergo cataract extraction, you will be faced with several choices. While cataract surgery has advanced tremendously in the last several years, most of the advances have had to do with the transformation of cataract surgery from a medical procedure to a refractive procedure. Cataract surgery can now allow patients to completely eliminate dependence on glasses for distance, intermediate and near.
During your visit, we will discuss the intraocular lens options and vision enhancements are available for your particular case.we will help you make the best decision, taking into account your lifestyle demands and hobbies as well and any other limitations.
Standard Monofocal IOLs
The standard monofocal IOL has been available for many years. It is also a good choice for those who are happy with wearing glasses after surgery. Although the standard monofocal IOL may reduce a patient's need for glasses, it is designed to replace the cataractous crystalline lens once it has been removed. The patient may expect improved distance vision with minimum correction or without glasses . For near vision patient will need corrective glasses.
They are of two types based on the design.
Single piece design – The central and peripheral portion are of the same material.
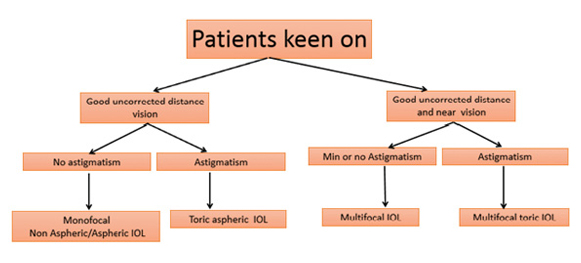
IOL Decision Making
Choosing an IOL is a difficult decision for any patient. The following flow chart is a simplified way of approaching about the question of which lens to implant.